Improving behavioral health outcomes through multidisciplinary research
The prevalence and severity of behavioral health issues, which includes mental illness and substance use disorders, has risen sharply in the United States. In 2021, more than 57 million Americans aged 18 or older reported the prevalence of mental illness in the last year, while 44.1 million met the criteria for having a substance use disorder.
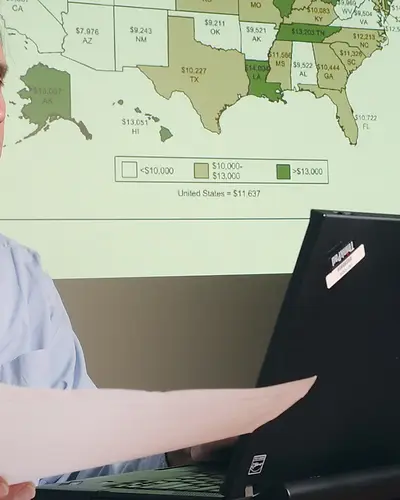
For several decades, RTI has collaborated with the Substance Abuse and Mental Health Administration (SAMHSA) on the National Survey on Drug Use and Health (NSDUH) to collect, analyze, and provide data around national estimates of mental illness and substance use disorders, as well as illicit drug, tobacco, and alcohol use.
Despite the rising numbers of individuals affected by mental illness and substance use disorders, utilization of behavioral health services remains low. The 2020 NSDUH report found that nearly 50% of respondents cited the inability to afford care as their most common reason for not seeking or utilizing behavioral health services. Many other factors contribute to the underutilization of services, including negative past experiences; stigma; lack of accessible, culturally competent providers; and other social factors.
Research into the Effectiveness of Behavioral Health Integration
Behavioral health integration is a potential remedy to this critical issue. It involves the collaboration of primary care physicians, behavioral health specialists, and specialty clinicians to create a person-centered care model that improves health outcomes. Our experts are evaluating the effectiveness of behavioral health integration models through the development of economic and epidemiological studies. RTI researchers are also working on creating, implementing, and evaluating behavioral health interventions.
Our research allows our federal partners to identify and implement data-driven solutions to improve our nation’s behavioral health along the full spectrum of care—including prevention, treatment, and intervention.
Evaluating the Impacts of Alternative Payment Models and Delivery System Change in Behavioral Health
RTI is a leader in evaluating the health and economic impacts of behavioral health alternative payment models. As the evaluators of the Centers for Medicare & Medicaid Services’ (CMS) State Innovation Models (SIM) Rounds 1 and 2, RTI conducted comprehensive mixed-methods evaluations of behavioral health integration. In SIM Round 1, behavioral health integration efforts in six states were catalyzed by strong working relationships and data sharing between behavioral health providers and primary care providers and the receipt of technical assistance to integrate care. However, bridging professional divides, lack of efficient and effective data sharing, and overcoming chronic behavioral health provider shortages hindered efforts to integrate care for Medicaid and Medicare enrollees. Maine's efforts to develop a behavioral health home model for their Medicaid enrollees with serious mental illness offered early lessons in integrating primary care within behavioral health and leveraging health information technology to improve delivery of behavioral health care. In SIM Round 2, three states implemented payment reform efforts to support behavioral health integration, leading to greater access to behavioral health care.
Assessing Substance Use Disorder and Innovations in Opioid Use Disorder Treatment
Recent research conducted by RTI experts highlights that almost 2 million Medicare beneficiaries had a past year SUD between 2015–2019. More than half of these beneficiaries were over the age of 65, and many did not receive any treatment for their SUD. Experts at RTI have conducted groundbreaking research into the prevalence of SUD in Medicare, as well as in-depth investigations to better understand barriers to accessing SUD treatments, such as prior authorizations, and the impacts this has on Medicare spending and utilization of acute care services. A recent evaluation report that RTI researchers contributed to provides the latest piece of evidence that providing high quality care for SUD in Medicare can improve economic and clinical outcomes for Medicare beneficiaries who have SUDs.
The rising prevalence of SUDs, serious mental illness (SMI), and serious emotional disturbance (SED) reflects a concerning trend in the United States. In 2015, 2017, and 2018, CMS issued guidance that states could apply for Medicaid section 1115 demonstration projects to transform the SUD and SMI/SED continuums of care for individuals enrolled in Medicaid. RTI is currently conducting a meta-analysis of the SUD and SMI demonstrations. This mixed-methods project leverages key informant interviews, Medicaid claims and national survey data analysis, and meta-analysis methods to identify patterns in implementation practices and demonstration impact in over 35 states. The goal is to determine which policies, program components, and contextual factors are related to success in improving access to treatment and reducing adverse health outcomes and costs.
Health Information Technology Adoption and Utilization in Behavioral Health Settings
Behavioral health providers (including both substance use disorder and mental health providers) lag behind physical health providers in adoption and use of health information technology (HIT) and health information exchange (HIE). RTI experts are at the forefront of supporting the U.S. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation in better understanding HIT adoption and utilization in behavioral health settings. In a two-phased project that first began with a literature review and focus groups with subject matter experts, RTI identified barriers to HIT adoption and interoperability among behavioral health providers—including concerns with patient confidentiality, cost, and gaps in technical training—and the policies that providers can leverage to improve use of HIT. In the second phase, which will be publicly released soon, RTI conducted case studies in six states to identify promising practices in electronic health record adoption and HIE participation among behavioral health providers in those states.
Related Projects
Medicaid Section 1115 SUD & SMI/SED Demonstrations: Addressing a Growing Crisis
Read More about Medicaid Section 1115 SUD & SMI/SED Demonstrations: Addressing a Growing Crisis