The prevalence of substance use disorders (SUD), serious mental illness (SMI), and serious emotional disturbance (SED) continues to grow over time. In 2022, an estimated 17% of people aged 12 and older had SUD, 6% of adults had SMI, and 8% of adults had a co-occurrence of any mental illness and SUD.
To address the public health crises associated with these conditions, the Centers for Medicare & Medicaid Services (CMS) introduced the Medicaid section 1115 SUD and SMI/SED demonstrations. Section 1115(a) of the Social Security Act enables state Medicaid programs to test changes in program eligibility, covered health care services, care delivery, and provider reimbursement, all while maintaining the overall goals of the Medicaid program. In 2015, 2017, and 2018, CMS issued guidance that states could apply for the SUD and SMI/SED Medicaid demonstrations to expand access to health care services for Medicaid enrollees with these conditions.
Medicaid Section 1115 SUD Demonstrations
The goals of the section 1115 SUD demonstrations are to:
- Raise rates of identification, initiation, and engagement in treatment.
- Increase treatment adherence and retention.
- Reduce overdose mortality.
- Decrease preventable or inappropriate emergency department and inpatient hospital utilization.
- Reduce preventable or inappropriate readmissions.
- Improve access to care for physical health conditions.
Generally, to receive approval for a section 1115 SUD demonstration, states must outline their plans for expanding access to multiple levels of evidence-based care for Medicaid enrollees with SUD and explain how inpatient and residential SUD services will coordinate with community-based recovery services. States with approved demonstrations can receive federal financial participation (FFP) for SUD treatment services provided in residential and inpatient facilities that qualify as institutions for mental diseases (IMDs).
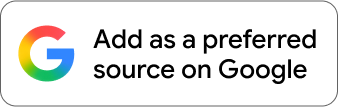
As of December 2024, 36 states and the District of Columbia (DC) have been approved to implement SUD demonstrations with the earliest state approved in 2016.
Medicaid Section 1115 SMI/SED Demonstrations
The goals of section 1115 SMI/SED demonstrations are to:
- Reduce utilization and length of stay in emergency departments.
- Reduce readmissions to acute care hospitals and residential settings.
- Improve availability of crisis stabilization, intensive outpatient, psychiatric hospital, and residential treatment setting services.
- Improve access to community-based services and integrated primary and behavioral health care.
- Improve care coordination and continuity of care after a hospitalization or residential treatment stay.
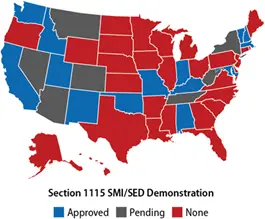
Section 1115 SMI/SED demonstrations also allow states to receive FFP for care delivered in an IMD as long as the state is taking action to ensure quality of care in IMDs and to improve access to mental health care for Medicaid enrollees with SMI or SED. States must also commit to maintaining funding levels for outpatient community-based mental health services. As of December 2024, 14 states and the DC have approved SMI/SED demonstrations, with the earliest state beginning implementation in 2019.
Medicaid Section 1115 SMI/SED Demonstrations
Evaluating how these demonstrations are improving access to and quality of SUD and SMI/SED services
In 2018 and 2023, CMS contracted with RTI to conduct state-level analyses and meta-analyses of the section 1115 SUD and section 1115 SMI/SED demonstrations. Meta-analyses identify variations in demonstration implementation and impact across states to determine the policies, program components, and contextual factors related to success in meeting demonstration goals. The project draws on qualitative and quantitative data, including
- Interviews with state Medicaid and behavioral health agency officials; IMD, residential care provider, and community mental health center leaders; and managed care organization representatives
- State demonstration documents, including implementation plans, state monitoring reports, and evaluation reports
- Fee-for-service and managed care Medicaid claims data from the Transformed Medicaid Statistical Information System
- National Survey of Substance Abuse Treatment Services and the National Substance Use and Mental Health Services Survey.
With these data, RTI is examining:
- State approaches and activities to achieve demonstration goals
- State experiences with demonstration implementation
- Perspectives of managed care and provider organizations
- SUD and mental health care service utilization and outcomes in demonstration states
Key Evaluation Findings of Medicaid Section 1115 Demonstrations for SUD and SMI/SED
Pre demonstration Measures of SUD Need, Treatment Use, Availability, and Outcomes Across States
Prior to the demonstration, SUD prevalence and treatment rates among Medicaid beneficiaries were higher in states that had an approved or pending section 1115 SUD demonstration by June 2020 than in states that did not have an approved or pending section 1115 SUD demonstration.
Prior to the demonstration, most demonstration states had opportunity for improvement in the availability of medication for opioid use disorder for beneficiaries receiving treatment in facilities.
How States Are Enhancing SUD Treatment Through Medicaid Demonstrations
Features of State Approaches to Improve Medicaid SUD Treatment Delivery Systems
More than three-quarters of the demonstration states included in the report added or expanded coverage of at least one SUD benefit category, most commonly recovery support, residential, and withdrawal management services.
Across the demonstration states featured, changes to meet residential medication assisted treatment (MAT) requirements and to residential treatment provider standards were common.
States Strengthen Medication Assisted Treatment Access
State Experiences Expanding Availability of Medication Assisted Treatment for Patients in Residential Settings
State officials described two approaches for ensuring provider adherence to the MAT requirements: adding requirements in residential provider standards and the Medicaid application/renewal process and implementing auditing and tracking.
Overcoming Implementation Challenges in Medicaid Section 1115 SUD Demonstrations
Implementation Challenges Across SUD States
States identified several common operational or administrative challenges that impacted implementation of section 1115 SUD demonstrations, including lack of provider knowledge about Medicaid structure, billing, and operational requirements; development of reimbursement rates for new residential levels of care; lack of provider familiarity with patient placement criteria; and operational challenges associated with utilization review.
States responded to challenges using several common strategies, including educating providers about Medicaid certification, billing practices, new patient placement criteria, and MAT; communicating early and often with providers to inform reimbursement rates; and expanding telehealth to address limited access to behavioral health professionals, especially in rural areas.