Insights
Powering a Faster Ebola Response in Kasaï with Digital Health Solutions

Dr. Bona (RTI) and Dr. Gaston Tsiapenda, the Deputy Ebola Incident Manager with the Ministry of Health, in front of the Bulape Health Zone office.
When Ebola emerged in the Democratic Republic of the Congo’s (DRC) Bulape and Mweka health zones in September 2025, the difference between worry and containment came down to one thing: whether frontline teams were prepared to collect, move, and use data—fast.
In some of the most remote corners of Kasaï Province of DRC, RTI International is working alongside the Ministry of Health through the Institute Nationale Sante Public (INSP) and Centre des opérations d’urgences de santé publique (COUSP), and partners to place one system—DHIS2—at the center of the response. That single alert sets off a chain: contacts to visit, homes to reach. A specimen is collected, given a unique ID, and tracked like a relay baton to the lab. Results flow seamlessly into DHIS2. Vaccination data joins the stream. And from a command dashboard, incident managers zoom from a bird’s-eye view of the outbreak down to the doorstep of the one contact still waiting.
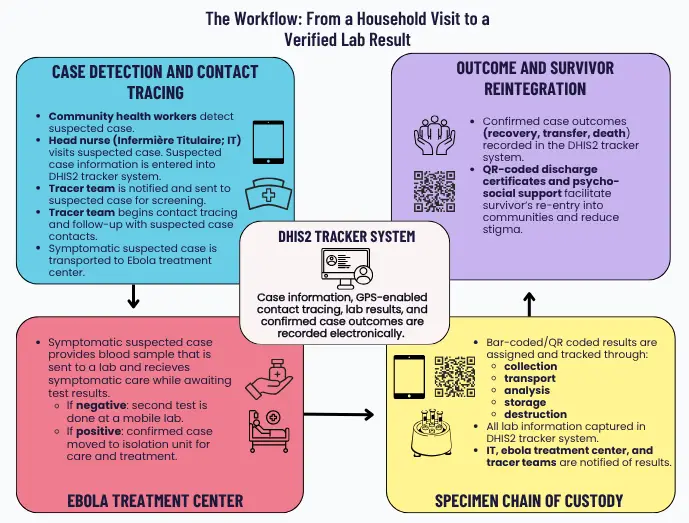
A note on the situation: As of September 28, 2025, MOH reported 53 confirmed and 11 probable Ebola cases concentrated in Bulape and Mweka. Of the confirmed cases there are currently 45 fatalities, and 5099 people have been vaccinated. There have been no new cases since September 26th. These figures change frequently as surveillance improves.
The Challenge: Last Mile Response in Places Without Roads or Grid Power
The outbreak in Kasaï is unfolding in health zones that are not only hard to reach but also hard to wire. This is a region where geography and infrastructure conspire against speed. Seasonal rains transform dirt tracks into deep mud, bridges are often nothing more than lashed logs, and the journey to a single village can involve a plane ride, followed by hours in a 4×4, then a motorcycle, and finally a canoe. These logistical hurdles mean that electricity is scarce, and reliable mobile phone service is a luxury—if it exists at all.
Such realities aren’t new. During earlier Ebola (EVD) responses in the DRC, responders documented multi-day treks from airstrips to outbreak epicenters, and coordination hubs cobbled together under tarps, powered by solar panels and satellite links. In Kasaï, these same constraints now collide with the urgency of outbreak control, making every kilometer a test of resilience and ingenuity. The remoteness doesn’t just slow down response—it shapes it, forcing teams to rethink supply chains, communication, and even basic surveillance in ways that urban health systems rarely imagine.
At the same time, the public health risk is real and quickly evolving. WHO’s Disease Outbreak News highlights both the severity of Ebola (case fatality rate of 64%) and the DRC government’s rapid declaration and mobilization in Bulape and Mweka. CDC situational updates emphasize that while the province’s remoteness may slow transmission, it also complicates access for responders.
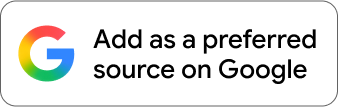
The Backbone: One DHIS2, Many Workflows
The DRC already uses DHIS2 as its national health information system and has deployed DHIS2 Tracker for epidemiologic surveillance (including mpox), demonstrating that data can be captured on Android tablets and measurably improve data timeliness and completeness. Building on that foundation, RTI and partners are configuring an EVD Tracker with stages for suspected case, contacts, laboratory, outcomes, and vaccinations. SMS alerts, dashboards, and maps are used by response teams and national level authorities to track progress and ensure that tracer teams and support are quickly sent to the right places. To strengthen outbreak preparedness, RTI and partners have designed a field first, offline capable package for health posts and tracer teams far from the electrical grid or cell towers.
Our goal is to get ≥80% of samples recorded with results in DHIS2, provide DRC’s emergency operation’s center called the COUSP with the tools and training to track contacts, reduce the spread and sustain automated situation reports (SITREPs) for incident managers—turning raw entries into decisions that can save lives.
The View: "30,000 Ft" Dashboard–and One Missed Contact
For COUSP, the DHIS2 Tracker system serves two vital functions at once:
- A high-level operational picture—an epi curve for Kasaï, case growth by health zone, laboratory turnaround times, and a heat map of investigations—so leadership can allocate resources, including teams and supplies.
- Clickthrough drilldown—from province to health zone to household—to see which contacts have missed follow-up visits, which alerts remain unvalidated, and where new hotspots may be emerging. This “last mile” visibility turns data into targeted door knocks that break transmission chains.
Behind the scenes, the team runs a data quality cycle (completeness, timeliness, accuracy) and holds surveillance–laboratory harmonization meetings to keep numbers aligned and actionable.
EVD Outbreak area (Yellow HZ) and Cordon (Orange HZ).
Powering the Response to Ebola: Starlink + Solar/Battery
Data can’t move if the network doesn’t exist. In Kasaï, Starlink terminals being used at Health Zone central health offices and mobile laboratory sites to create reliable sync windows and nightly coordination calls where mobile coverage is patchy or absent.
Power can’t fail if labs and data entry are to keep pace. The project includes energy audits and the procurement/installation of photovoltaic panels, batteries, and inverters at priority sites, plus maintenance training and remote monitoring. This ensures that epidemiological teams, tracers, and laboratory teams can keep working after dusk or during grid outages. Phases one and two of the project target eight priority installations.
These are not luxuries; they are enablers. RTI’s previous experience supporting outbreaks in Guinea (2014) and DRC (2017) documented how quickly installed satellite equipment and solar arrays made coordination possible in the outbreak epicenter when the grid didn’t reach and generators ran only part-time.
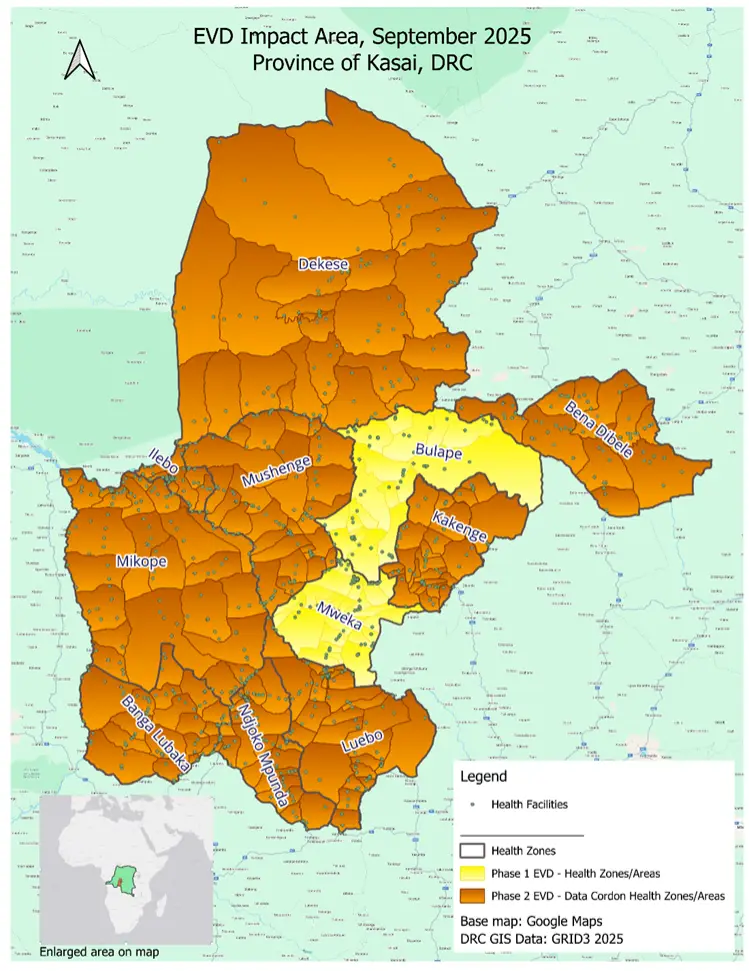
Building Local Capacity at Scale to Strengthen Global Health Security
A cornerstone of this response is empowering the DRC’s own public health workforce—not just with technology, but with the skills, confidence, and ongoing support to lead the fight against Ebola now and in the future.
Supporting COUSP in the Field:
RTI is working side-by-side with the COUSP and local health authorities, ensuring they have the resources, technical guidance, and on-the-ground backup needed to carry out critical fieldwork—from household investigations to specimen tracking and data-driven decision-making. Our teams help COUSP troubleshoot challenges in real time, adapt workflows to local realities, and ensure that every new tool or process fits the context of Kasaï’s remote health zones.
Capacity Strengthening Across the Health System.
But training is just the start. Ongoing mentorship and on-site problem solving are built into the response. RTI works with local partners to provide refresher sessions, field supervision, and rapid-response technical support—so that as new challenges arise, local teams have the confidence and backup to solve them. This approach ensures that quality is sustained long after the initial rollout, and that the DRC’s public health workforce emerges stronger, more resilient, and ready to lead future responses.
The result: A growing cadre of Congolese professionals—supported, mentored, and equipped—who are not only responding to today’s outbreak, but building the foundation for a healthier, more secure future for their communities and for global health security.
How This Work Aligns with Current U.S. Global Health Priorities
Detecting and containing outbreaks at their source helps minimize the risk of cross-border spread and the broader social and economic disruptions that can follow. This response emphasizes a country-led model: supporting frontline health workers, investing in locally managed data systems like DHIS2, and using clear performance benchmarks to guide ongoing improvements. Leveraging proven technologies—from secure digital platforms to resilient connectivity and power solutions—ensures that surveillance, laboratory, and coordination activities continue even in the most remote settings. Direct funding to the COUSP—paired with collaborative stewardship—accelerates financial skill development and strengthens the financial capacity of local government partners.
These strategies reflect the direction outlined in recent U.S. global health guidance, which prioritizes early detection, rapid response, and timebound cooperation.
Knowing precisely where the Ebola virus is circulating—and tracking every infection and specimen—also strengthens biosecurity. By maintaining a transparent, real-time record of cases and samples, the system reduces the risk that infectious materials could be diverted or misused by nefarious actors. This level of oversight not only protects local communities but also contributes to broader efforts to prevent the intentional spread or exploitation of dangerous pathogens.
What Success Looks Like: Faster Confirmations and Stronger Digital Health Systems
- Faster confirmations: Specimen to result times drop because the sample journey is tracked and timely and accurate laboratory results post directly into DHIS2.
- Complete follow-up: COUSP can see who has not yet been visited and deploy surge teams to close gaps.
- Quality assured: Routine checks for punctuality, completeness, and accuracy keep the data trustworthy, while harmonization meetings prevent surveillance–lab mismatches.
- Sustained operations: Starlink connectivity combined with solar panels and battery backup ensures uninterrupted data synchronization and keeps laboratories and decision centers online during power outages and after dark.
Beyond these indicators are the human outcomes: a tracer team making a final follow-up visit on a motorbike before dusk; a lab technician posting a positive result that triggers more intense monitoring; or a survivor walking home with an official QR coded discharge certificate that helps counter stigma.
The Road Ahead: Scaling Digital Health Solutions for Future Ebola Responses
The immediate priority is to work with our government partners at COUSP to stabilize Bulape and Mweka and then scale to additional at-risk zones surrounding the outbreak area in Kasaï and neighboring Sankuru through connectivity, solarization, and training milestones. Outbreak preparedness hinges on scalable, resilient systems. That's why the foundation will continue to be a single, country-owned system of record (DHIS2) that gives local leaders the right data at the right time to stop transmission.
In places where roads wash out and power grids end, data still has to move. By pairing tablets with people and an offline first DHIS2 and backstopping the last mile with Starlink and solar, the Bulape–Mweka response demonstrates how to make that happen while protecting Congolese families today and keeping America safer.
Learn More
Disclaimer: This piece was written by Daren Trudeau (Senior Health System Strengthening Specialist ), Bonaventure Ngoyi (Field Epidemiologist), and Lavanya Gupta (Research Public Health Analyst) to share perspectives on a topic of interest. Expression of opinions within are those of the author or authors.