In public health research, suicide has emerged as a critical challenge, impacting people across races, ethnicities, and age groups. According to the Centers for Disease Control and Prevention, nearly 50,000 individuals died by suicide in 2022—roughly 1 death every 11 minutes. These rates were higher for individuals who thought about or had attempted suicide previously. In addition, research has shown that 83% of individuals who died by suicide have visited a primary care provider in the prior year, and 50% have visited that provider within 30 days of their death. Although suicide is preventable, it will take a multidisciplinary, multi-organization approach to create the policies and programs needed to improve our suicide prevention efforts in the United States.
The Zero Suicide model aims to reduce the risk of suicide for all individuals seen in health care systems
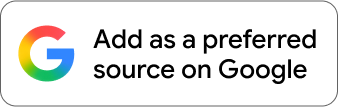
From 2010 through 2013, the National Action Alliance for Suicide Prevention, the Suicide Prevention Resource Center, and other national suicide prevention experts developed and launched the Zero Suicide in Health and Behavioral Health Care Model. The Zero Suicide Initiative (ZSI) is one of many approaches to suicide prevention. The foundational principle of ZSI is that behavioral health systems should have the infrastructure, policies, procedures, and staff that are trained to ensure that there are zero deaths by suicide. The ZSI model is operationalized by adopting and implementing a holistic approach, embodied through seven core elements—Lead, Train, Identify, Engage, Treat, Transition, and Improve (Figure 1). These core elements inter-relate and serve to guide health systems in their care for individuals with suicidal thoughts and urges.
Figure 1. Seven ZSI Elements
Source: RTI International
Similar to other clinically oriented interventions, ZSI relies on an approach that screens patients to identify their needs, connects patients to care, and provides evidence-based treatment and care transition support. Figure 2 outlines the clinical pathway used by the ZSI model:
- Patients receive screening and assessment to identify whether they are at risk as part of the Identify element.
- Patients are then engaged in collaborative care aimed at addressing their level of risk identified during the screening and assessment process (Engage element).
- These individuals also receive support as part of evidence-based, culturally appropriate treatment and care (Treat element).
- Patients may be transitioned out of care or between care settings while maintaining their connection to providers who are working with them to reduce their risks of suicide and strengthen protective factors around them (Transition element).

Figure 2. Clinical Care Pathway to Suicide Care
Source: RTI International
Non-Hispanic American Indian/Alaska Native communities experience higher suicide rates
American Indian/Alaska Native (AI/AN) communities have one of the fastest-growing rates of suicide in the United States. Recent data from the National Violent Death Reporting System show a nearly 20% rise in the rate of death by suicide among AI/AN communities. Even more staggering is that rates of death by suicide among AI/AN males increased by 71% from 1999 to 2017 compared to 26% among males of all other racial and ethnic groups.
To address these alarming trends, the Indian Health Service (IHS) have supported the implementation of the Zero Suicide Initiative in IHS-area sites for the past decade. Their Zero Suicide efforts have provided interrelated resources, including AI/AN Zero Suicide Academies, Communities of Learning, and Tailored Technical Assistance. Additionally, the Substance Abuse and Mental Health Services Administration and the National Institute of Mental Health have established a number of grant programs to fund Zero Suicide Implementation in health care systems. Across all these funding mechanisms, more than 40 health care systems or grantees have been awarded funds. Since 2023, RTI—with funding from IHS—has been serving as a ZSI Coordinating Center to support IHS-funded ZSI grantees.
Lessons learned from implementing Zero Suicide Initiative
In partnership with the Office of the Assistant Secretary for Planning and Evaluation, RTI developed a detailed report examining the implementation and sustainability practices of organizations operationalizing ZSI in 2021. From this report, Implementing and Sustaining Zero Suicide: Health Care System Efforts to Prevent Suicide Report, four key lessons emerged:
- Strong leadership and management is critical to ZSI implementation progress. Leadership is typically responsible for managing and promoting the ZSI programming to ensure that communication is coordinated across staff and to develop policies, processes, and practices for suicide prevention and intervention.
- Establishing champions and dedicated staff across organizations helps facilitate implementation. Staff involvement in a steering or an implementation group helped ZSI implementation and led to more coordinated approaches, policies, and communication.
- Advanced electronic health record (EHR) systems are essential for tracking suicide-related activity, reviewing suicide prevention efforts, and monitoring quality improvement. Modern EHRs that can consistently track patient care, suicide risk screening and assessment results, and safety plans help providers efficiently care for patients at risk of suicide. EHR capacity can ensure that data and information are easily accessible in a timely manner to inform and share information across providers.
- Diversifying funding, maintaining fidelity to ZSI protocols and practices, and building strategic community partnerships were found to be key components for sustaining ZSI. Organizations that leveraged internal and external funding were able to sustain their Zero Suicide efforts. In particular, organizations approached investments (e.g., training costs, EHR modifications, hiring staff) on an as-needed basis, pursued federal grants, held annual fundraisers, and developed partnerships with states to receive additional state and federal funds to continue. Organizations also developed and followed ZSI protocols and practices to maintain fidelity to Zero Suicide following implementation. Finally, establishing a network of community partnerships has helped build momentum for implementation and ensure that suicide prevention becomes part of the community’s identity.
Zero Suicide Implementation requires effective rollout through coordinated communication and leadership support, adoption of and fidelity to policies and protocols, advanced EHR systems for tracking suicide-related activity and monitoring quality improvement, and strategies to ensure that the program is impactful and sustainable in the long term. These four lessons highlight that a multifaceted approach is required for effective suicide prevention in Indian country. Equipped with these insights, RTI continues to support organizations implementing ZSI to ensure that the number of deaths by suicide in these communities is zero.
Learn more about RTI’s data-driven research on effective suicide prevention and our expertise managing multicenter research and collaborative research networks.