Traditional Approaches to Public Health Surveillance
Surveillance of public health behaviors and health status, including chronic and infectious diseases and other health conditions, has traditionally been conducted through large, nationally representative surveys. New methods for obtaining some of the data traditionally acquired through these surveys, such as through EHRs, hold promise. In Toward a 21st Century National Data Infrastructure: Enhancing Survey Programs by Using Multiple Data Sources, the capture of important survey data from other sources, like EHR data, is one dimension of a broader effort. With stagnant or shrinking budgets potentially limiting the reach and quality of many surveys, new methods for collecting even a subset of these data are gaining increased attention. This approach is one of many ongoing contributions to a much larger effort to advance a national health data infrastructure.
Emerging Role of EHRs in Data Collection
Significant advances in collecting and using EHR data, supported by standards like Health Level-7 (HL7) Fast Health Care Interoperability Resources (FHIR) and governance changes such as the Trusted Exchange Framework and Common Agreement (TEFCA), have the potential to provide real-time access to at least a portion of the data currently obtained through health surveys. As these capabilities evolve, large surveys are increasingly exploring the potential of EHR data to complement—and in some cases, replace—data gathered through traditional, more labor-intensive survey methods.
Advantages of Using EHR Data for Public Health Surveillance
EHR data offer three advantages over traditional survey data:
- Timely: A survey wave can take several months from initial survey preparation to final data capture, with some additional months required for data cleaning and analysis. Establishing relationships with health care facilities and communities, securing data-sharing agreements, and establishing transfer mechanisms for EHR data acquisition can be time-consuming, but this investment often enables data to be received within weeks, rather than months or years.
- Cost-Effective: Surveys require data collection staff, field visits, and follow-up, which are costly, particularly as sample sizes grow. EHR data are already being collected for other purposes, so data collection expenses are relatively low.
- Detailed: Surveys must consider respondents’ time and attention and are subject to biases (e.g., recall bias) that can influence the accuracy and completeness of participants’ answers. The amount of information contained in EHR data would not be reasonable to ask a respondent due to time constraints or memory limitations. EHR data—although not free from bias—are generally more comprehensive and, in some cases, span the participants’ entire medical history. EHR data may also include information on health events that may be sensitive and difficult to collect directly, without additional emotional or time burden on respondents.
Advantages of Survey Data and Disadvantages of EHR Data
Although EHR data offer some advantages over traditional survey data, some gaps remain. EHR data are inconsistently available, sometimes erroneous, and limited in scope. Survey data can be used to validate, augment, and supplement real-time data collection methods where higher accuracy and validity are desired:
- Validation: Traditional surveys can ensure quality and consistency through quality control methods at the point of questioning or through follow ups with respondents. EHR data are much harder to correct after they have been collected.
- Augmentation: Surveys allow for the collection of non-standard data or data that are collected beyond the scope of an EHR. For example, detailed employment data, health care attitudes and preferences, income, and measures of health care access are often not captured in an EHR but may be important to obtain.
- Supplementation: People who cannot access or do not use health care are likely to be missing from EHR-based data collection and may be more easily captured through traditional survey methods. For example, uninsured populations often have inconsistent health care access, resulting in missing or incomplete records that could bias estimates derived from EHR data.
Complementary Roles of Survey and EHR Data in Public Health Surveillance
Survey data remain crucially important in the public health data landscape, offering insights not collected from EHR data sources, such as peoples’ beliefs and behaviors in specific contexts. Although there are ongoing projects are examining the use of sources like EHRs to enhance survey data collection (e.g., the Gravity Project), available EHR data on behaviors and context are sparse and incomplete. Compared with systemic EHR data collection efforts, surveys can respond faster to changes in current events or scientific developments by adding a new module or modifying questions, an adaptation that is difficult to implement quickly across administrative systems like EHRs. Therefore, although EHR data can be timelier, cheaper, and more complete in some contexts, they fall short in others. Agencies must thoughtfully consider which type of longitudinal data collection efforts are best suited to answer their public health questions. In the long run, agencies will see the most return on investment by finding synergistic ways to integrate survey and EHR data.
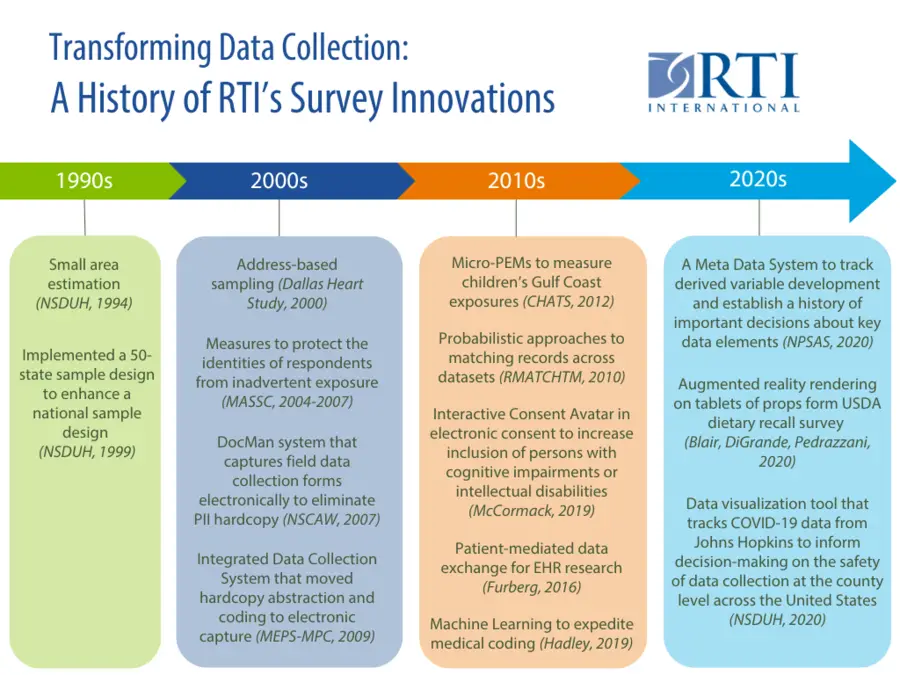
As an industry leader in survey administration, data collection, (bio)statistics, data science, and health informatics, RTI International is well-positioned to support health care surveys as they expand to a new, hybrid format that includes trusted survey methods and novel approaches for incorporating EHR data.
Case Studies: Centers for Disease Control and Prevention’s (CDC’s) Real-World Applications of EHR Data Integration
CDC’s series of National Health Care Surveys exemplify traditionally conducted surveys that are transitioning, either completely or in part, to EHR data collection. These surveys, ongoing since the 1960s, assess health care services and utilization. Several have begun incorporating EHR data in addition to or instead of the traditional fielded surveys.
National Ambulatory Medical Care Survey (NAMCS)
RTI leads the provider component of NAMCS, conducted through a traditional survey model. In recent years, the full NAMCS program has expanded to include three components—a patient survey, a physician interview, and a community health center administrator/provider interview—with EHR-derived data incorporated into two of these components. As projects like NAMCS are transitioning to new data collection methods, RTI is helping CDC understand the challenges and opportunities of using EHR data.
National Post-acute and Long-term Care Study (NPALS)
NPALS provides statistical information on the major sectors of paid, regulated long-term care services in the United States. With the increasing adoption of EHR systems for similar surveys conducted in other settings, there is a growing interest in modifying NPALS survey data collection methods. In a major step toward this shift, CDC contracted with RTI to assess the feasibility of this transition. RTI evaluated the potential for extracting NPALS data elements from commercial EHR platforms used by residential care communities and adult day service centers, aiming to augment and streamline survey data collection processes.
Multi-state EHR-based Network for Disease Surveillance (MENDS)
Funded by CDC and led by the National Association of Chronic Disease Directors (NACDD), MENDS uses EHR data from across the United States for chronic disease surveillance. Because chronic diseases do not typically require reporting to public health authorities, population-based surveys, such as CDC’s Behavioral Risk Factor Surveillance System (BRFSS), have been used to estimate the prevalence and incidence of these conditions. The goal of MENDS is to compile detailed information on conditions like diabetes, hypertension, and obesity to support public health prevention and planning efforts.
RTI collaborated with NACDD to evaluate existing MENDS processes and explore opportunities for data modernization. This evaluation highlighted the high value proposition of EHR-based surveillance, with partners eager to participate due to its potential benefits, like reduced labor costs and improved efficiency in data collection methods. However, scaling this approach presents challenges, such as the need for substantial information technology (IT) infrastructure to support chronic disease surveillance within and between health systems and public health authorities. Other limitations include the lack of standardization in source data systems and EHRs, as well as the early real-world implementation of standards like FHIR. RTI recommended that MENDS take an incremental approach, adopting what works today while incorporating more modern processes as infrastructure and standards mature.
National Health and Nutrition Examination Survey (NHANES)
NHANES and CDC have always prioritized accessibility to accomplish their goal of collecting a comprehensive dataset that is representative of the U.S. population. RTI, the current data collection contractor for NHANES, is collaborating with CDC to design a new fleet of customized mobile examination centers that offer greater mobility and flexibility than previous iterations. This shift toward increased flexibility presents an opportunity to consider new ways to collect comprehensive data on these participants.
NHANES’ data collection and laboratory protocols—including anthropometrics and biospecimen collection—are considered the gold standard in their field. Additionally, NHANES is the largest and most representative survey that collects data completely outside of the traditional medical system. Because no data are pulled from EHR records, this dataset represents an important replication and validation opportunity for comparison with EHR datasets of similar populations in the United States. Furthermore, the resource investment to collect new samples and data from each participant could be supplemented by EHR data with relatively little additional burden on participants.
Looking Ahead: RTI’s Vision for Health Data Modernization
RTI continues to drive innovations in health data collection and integration to reduce the complexity of public health data exchange. For example, RTI conducted a preliminary study on hospitals’ ability to extract and submit Medical Expenditure Panel Survey (MEPS) Medical Provider Component (MPC) data electronically using EHR and financial systems sources and to identify the most convenient way for hospitals to extract and submit the data. RTI is conducting work with wearables and sensors, in part being responsive to efforts to support the collection of patient-generated health data.
Explore data modernization solutions driving the advancement of public health surveillance.